Last Updated on December 15, 2024 by Michelle Wan
Blood clots, while a natural part of the body’s healing process, can sometimes form inappropriately, leading to serious health complications. Conditions like deep vein thrombosis (DVT), pulmonary embolism (PE), or even strokes can occur when clots block critical blood flow. The good news is that proper awareness and proactive measures can be helpful in preventing blood clots.
This guide provides detailed insights into the causes of blood clots, risk factors, prevention strategies, and when to seek medical help.
Understanding Blood Clots
A blood clot is a gel-like mass formed by platelets and fibrin in the blood to stop bleeding. While clots are essential for healing injuries, they can be dangerous if they:
- Form when they’re not needed.
- Do not dissolve naturally.
- Travel through the bloodstream and block vital arteries or veins.
Common Types of Dangerous Blood Clots
Deep Vein Thrombosis (DVT):
A clot forms in a deep vein, usually in the legs and the symptoms include swelling, redness, and pain in the affected area.
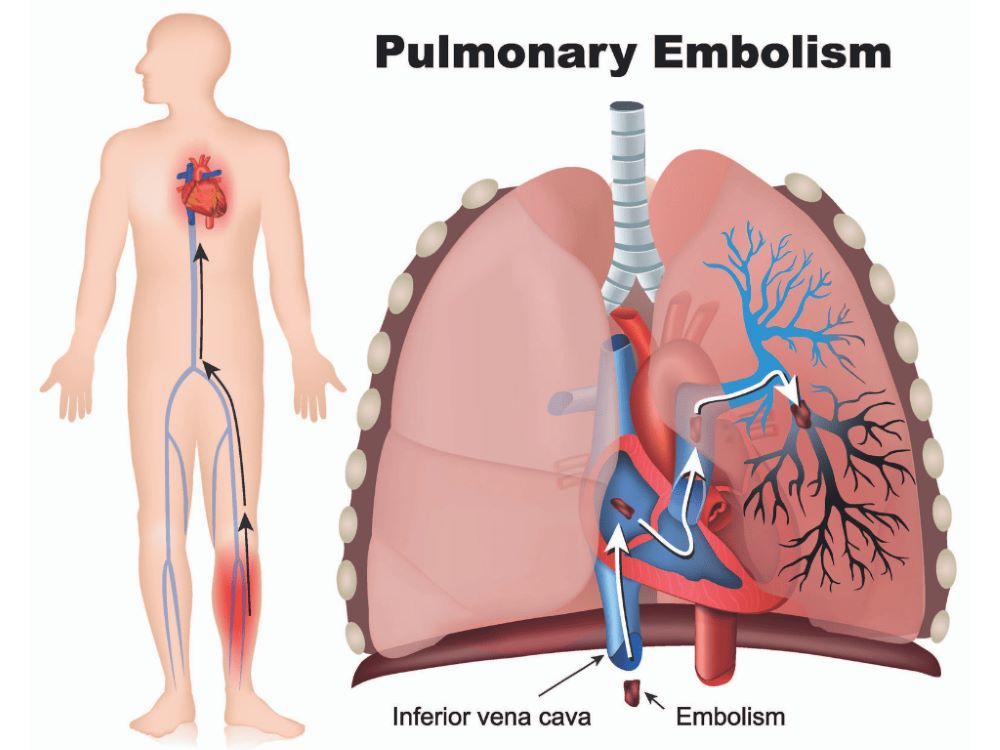
Pulmonary Embolism (PE):
Occurs when a clot travels to the lungs, blocking blood flow and symptoms include shortness of breath, chest pain, and rapid heart rate.
Arterial Thrombosis:
A clot forms in an artery, potentially leading to a heart attack or stroke and symptoms depend on the location of the blockage but often include severe pain and sudden loss of function.
Causes of Blood Clots
Several factors can trigger abnormal blood clot formation, including:
- Immobility: Prolonged sitting or lying down reduces blood flow, increasing clot risks.
- Injury or Surgery: Tissue damage can activate clotting mechanisms.
- Medical Conditions: Conditions like cancer, diabetes, and heart disease can elevate clot risks.
- Pregnancy: Hormonal changes during pregnancy increase clotting factors.
- Medications: Certain birth control pills, hormone replacement therapies, and chemotherapy drugs can heighten clot risks.
Risk Factors for Blood Clots
While anyone can develop a blood clot, some individuals face higher risks. Key risk factors include:
- Age: Risk increases with age, especially after 60.
- Family History: A history of clotting disorders increases susceptibility.
- Obesity: Extra weight puts pressure on veins, slowing blood flow.
- Smoking: Damages blood vessels and increases clotting risk.
- Inactivity: Long flights, bed rest, or recovery periods can lead to reduced blood circulation.
Preventing Blood Clots
Prevention begins with awareness and adopting lifestyle changes or medical interventions suited to your individual risk level. Here are proven strategies to reduce your chances of developing blood clots:
Stay Active
- Regular Exercise: Engage in activities like walking, swimming, or cycling to improve circulation.
- Avoid Prolonged Sitting: Stand, stretch, or move every hour, especially during long flights or workdays.
Maintain a Healthy Weight
- Weight management reduces pressure on your veins and decreases the risk of DVT.
Stay Hydrated
- Dehydration thickens blood, making clots more likely. Drink plenty of water throughout the day.
Quit Smoking
- Smoking damages blood vessels, increasing clot risks. Seek support to quit and protect your vascular health.
Wear Compression Stockings
- For individuals at higher risk, compression stockings improve blood flow in the legs and reduce the chance of clot formation.
Medications for High-Risk Individuals
- Anticoagulants (Blood Thinners): Prescribed for people with a history of clots or other risk factors. These include medications like warfarin or direct oral anticoagulants (DOACs).
- Aspirin Therapy: May be recommended in low doses for clot prevention in certain cases.
Post-Surgery or Bed Rest Prevention
- Early Mobilization: Get up and move as soon as medically possible after surgery or prolonged bed rest.
- Intermittent Pneumatic Compression Devices: Often used in hospitals to improve circulation during recovery.
Recognizing the Warning Signs of a Blood Clot
It’s crucial to recognize early symptoms of a blood clot to seek immediate medical attention. Symptoms vary depending on the location of the clot but may include:
- DVT: Swelling, redness, warmth, or pain in the leg or arm.
- Pulmonary Embolism: Sudden shortness of breath, chest pain, coughing (possibly with blood), or a rapid heart rate.
- Stroke: Sudden numbness, weakness, confusion, difficulty speaking, or loss of coordination.
- Heart Attack: Chest pain, shortness of breath, nausea, or lightheadedness.
If you or someone you know experiences these symptoms, seek emergency medical care immediately.
When to See a Doctor
You should consult a healthcare provider if you:
- Have a family history of blood clots or clotting disorders.
- Experience unexplained swelling, pain, or redness in a limb.
- Are scheduled for surgery and want to discuss preventive measures.
- Are pregnant or using hormonal therapies and concerned about clot risks.
How Medical Malpractice Can Lead to Preventable Blood Clots
In some cases, blood clots occur due to medical negligence, such as:
- Failure to Diagnose: Delayed identification of clot risk factors.
- Improper Post-Surgical Care: Neglecting preventive measures like compression devices or early mobilization.
- Medication Errors: Incorrect dosage or failure to prescribe anticoagulants for high-risk patients.
If medical malpractice contributed to a blood clot, families may be eligible to seek compensation to cover medical expenses, long-term care, and emotional distress.
Blood clots are a serious medical concern, but with the right lifestyle changes, awareness, and preventive care, they can often be avoided. By staying informed and proactive, you can significantly reduce your risk of developing dangerous clots.
If you suspect medical negligence led to a preventable blood clot or health complication, contact Thomas & Wan LLP for a free consultation. Our experienced attorneys are here to help you understand your legal options and secure the justice and support you deserve.